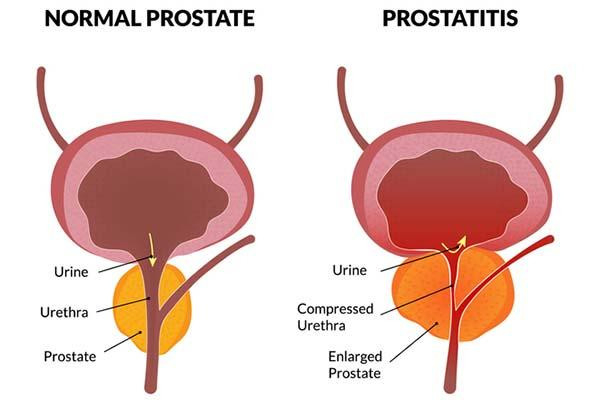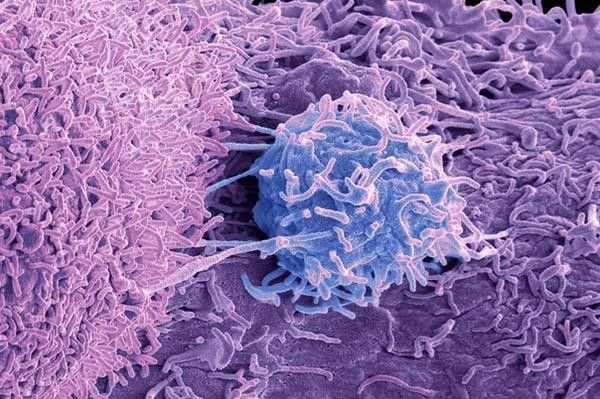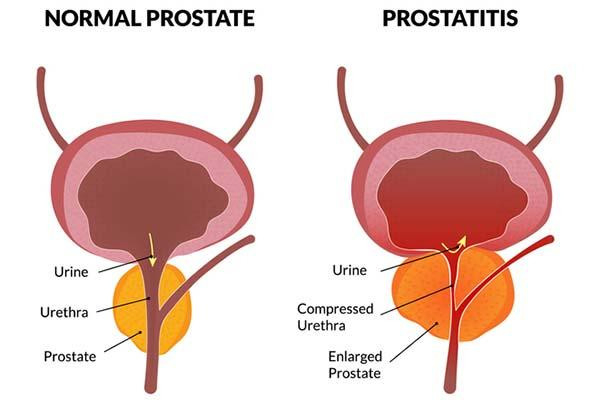
Prostatitis, or inflammation of the prostate, is more common than you might think — it accounts for roughly two million doctor visits every year. The troubling symptoms include burning or painful urination, an urgent need to go (especially at night), painful ejaculations, and also pain in the lower back and perineum (the space between the scrotum and anus).
Prostatitis overview
There are four general categories of prostatitis:
Acute bacterial prostatitis comes on suddenly and is often caused by infections with bacteria such as Escherichia coli that normally live in the colon. Men can suffer muscle aches, fever, and blood in semen or urine, as well as urogenital symptoms. Acute inflammation can cause the prostate to swell and block urinary outflow from the bladder. A complete blockage is a medical emergency that requires immediate treatment. Depending on symptom severity, hospitalization may be necessary.
Chronic bacterial prostatitis results from milder infections that sometimes linger for months. It occurs more often in older men and the symptoms typically wax and wane in severity, sometimes becoming barely noticeable.
Chronic nonbacterial prostatitis, also called chronic pelvic pain syndrome (CPPS), is the most common type. CPPS can be triggered by stress, urinary tract infections, or physical trauma causing inflammation or nerve damage in the genitourinary area. In some men, the cause is never identified. CPPS can affect the entire pelvic floor, meaning all the muscles, nerves, and tissues that support organs involved in bowel, bladder, and sexual functioning.
Asymptomatic inflammatory prostatitis is diagnosed when doctors detect white blood cells in prostate tissues or secretions in men being evaluated for other conditions. It generally requires no treatment.
Both acute and chronic bacterial prostatitis can cause blood levels of prostate-specific antigen (PSA) to spike. This can be alarming, since high PSA is also indicative of prostate cancer. But if a man has prostatitis, then that condition — and not prostate cancer — may very well be the reason for the rise in PSA.
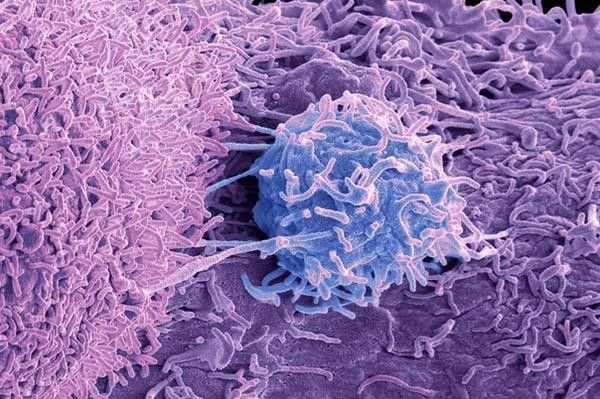
Prostatitis treatments
Fortunately, research advances are leading to some encouraging developments for men suffering from this condition.
Antibiotics called fluoroquinolones are effective treatments for acute and chronic bacterial prostatitis. A four-to six-week course of the drugs typically does the trick. However, bacterial resistance to fluoroquinolones is a growing problem. An older drug called fosfomycin can help if other drugs stop working. PSA levels will decline with treatment, although that process may take three to six months.
CPPS is treated in other ways. Since it is not caused by a bacterial infection, CPPS will not respond to antibiotics. Medical treatments include nonsteroidal anti-inflammatory drugs such as ibuprofen, alpha blockers including tamsulosin (Flomax) that loosen tight muscles in the prostate and bladder neck, and drugs called PDEF inhibitors such as tadalafil (Cialis) that improve blood flow to the prostate.
Specialized types of physical therapy can provide some relief. One method called trigger point therapy, for instance, targets tender areas in muscles that tighten up and spasm. With another method called myofascial release, physical therapists can reduce tension in the connective tissues surrounding muscles and organs. Men should avoid Kegel exercises, however, which can tighten the pelvic floor and cause worsening symptoms.
Acupuncture has shown promise in clinical trials. One study published in 2023 showed significant improvements in CPPS symptoms lasting up to six months after the acupuncture treatments were finished. Mounting evidence suggest that CPPS should be treated with holistic strategies that also consider psychological factors.
Men with CPPS often suffer from depression, anxiety, and other mental health issues that can exacerbate pain perception. Techniques such as mindfulness and cognitive behavioral therapy for CPPS can help CPPS sufferers develop effective coping strategies.
Comment
“An accurate diagnosis is important given differences in how each of the four categories of prostatitis is treated,” said Dr. Boris Gershman, a urologist at Beth Israel Deaconess Medical Center and assistant professor of surgery at Harvard Medical School. PSA should also be retested after treating bacterial forms of prostatitis, Dr. Gershman added, to ensure that the levels go back to normal. If the PSA stays elevated after antibiotic treatment, or if abnormal levels are detected in men with nonbacterial prostatitis, then the PSA “should be evaluated in accordance with standard diagnostic approaches,” Dr. Gershman said.
About the Author

Charlie Schmidt, Editor, Harvard Medical School Annual Report on Prostate Diseases
Charlie Schmidt is an award-winning freelance science writer based in Portland, Maine. In addition to writing for Harvard Health Publishing, Charlie has written for Science magazine, the Journal of the National Cancer Institute, Environmental Health Perspectives, … See Full Bio View all posts by Charlie Schmidt
About the Reviewer
Marc B. Garnick, MD, Editor in Chief, Harvard Medical School Annual Report on Prostate Diseases; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Marc B. Garnick is an internationally renowned expert in medical oncology and urologic cancer. A clinical professor of medicine at Harvard Medical School, he also maintains an active clinical practice at Beth Israel Deaconess Medical … See Full Bio View all posts by Marc B. Garnick, MD